What is the Cornea
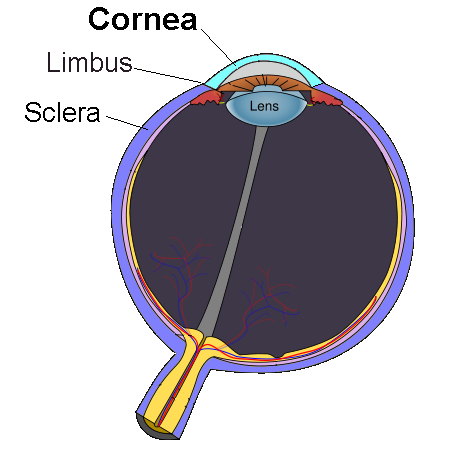
The cornea is the clear window at the front of the eye. Its function is to focus light on the back of the eye to enable the eye to see in focus. Diseases of the cornea that affect its shape and transparency can lead to blurring of vision. Other common complaints in people with corneal conditions are discomfort or pain, redness of the eye and light sensitivity. The most common condition that causes sight loss from altering the shape of the cornea is called keratoconus. Loss of transparency of the cornea is most commonly caused by diseases of its inner lining, such as Fuchs corneal dystrophy, and inflammatory conditions and infections that lead to haziness or scarring of the cornea.
Management of corneal disease
Most corneal conditions are managed medically, in other words with drops and tablets. The mainstay of surgical treatment of corneal disease is corneal transplantation, where the cornea of a deceased donor is transplanted to improve sight. The type of corneal transplant performed depends on the condition being treated.
For diseases of the inner lining of the cornea (Fuchs dystrophy, bullous keratopathy), DMEK (Descemet’s Membrane Endothelial Keratoplasty) is typically performed. In this procedure only the inner lining of the cornea, called the endothelium, is replaced.
Conditions affecting the stroma, the normally clear central layer of the cornea, are managed by DALK (Deep Anterior Lamellar Keratoplasty), which involves replacing the middle and front layers, leaving the healthy endothelial layer at the back of the cornea in place. Keratoconus is the commonest indication for DALK. Corneal transplantation is highly successful in the vast majority of patients and leads to a significant improvement in vision and quality of life.
Another common corneal procedure is called corneal crosslinking. This is performed to prevent progression in keratoconus. If keratoconus is detected early enough, sight can be preserved for life with this treatment. Only 1 in 200 patients requires repeat corneal crosslinking based on our experience of treating our first 1500 patients. Corneal crosslinking represents one of the most important advances in ophthalmology over the past 15 years.
What are the indications for corneal transplantation
A variety of conditions can lead to irregularity, scarring or waterlogging of the cornea. When this occurs, the only solution might be a corneal transplant.
A corneal transplant may be performed to:
- Improve sight,
- Alleviate pain, or
- Repair a perforation (if your cornea has ruptured)
Corneal transplant procedure
Patients undergoing corneal transplantation are admitted to hospital on the day of the operation and may be discharged home on the same day or kept overnight in the hospital.
Corneal transplants are either full thickness or partial thickness. For a full thickness transplant, called a PK or Penetrating Keratoplasty, the centre of the cornea is fully removed. It is replaced by a disc of healthy cornea from the donor eye which is stitched into the patient’s eye. The operation takes about an hour and is usually performed under general anaesthesia
Partial thickness transplants are used to replace the abnormal layers of the cornea only. A DALK or Deep Anterior Lamellar Keratoplasty is performed to replace the abnormal front layers of the cornea, leaving the back healthy layer intact. The donor’s front layer of the cornea is stitched into the back layer of the cornea. This operation takes about and hour and a half and is usually performed under general anaesthesia.
DSEK, short for Descemet’s Stripping Endothelial Keratoplasty, and DMEK or Descemet’s Membrane Endothelial Keratoplasty, are operations that remove the back layer of your cornea, the endothelium, and replace it with healthy donor tissue. There are very few sutures used in DMEK and DSEK and instead a small air bubble injected inside the eye holds the transplanted tissue in place. These operations are usually performed under local anaesthesia and take about 30-40 minutes.
The choice of full or partial thickness corneal transplants depends on many factors. The best operation is chosen based on the patient’s individual needs so that it has the highest chance of success.
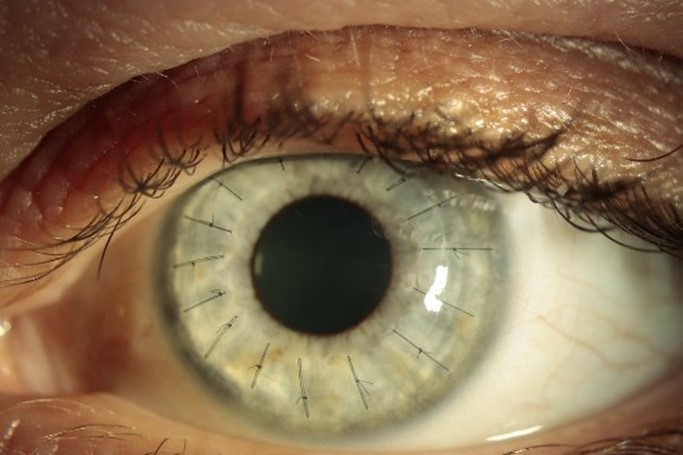
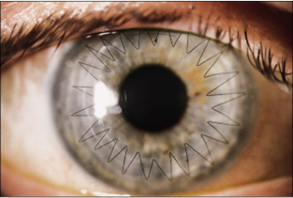
The appearance of the eye after DALK. The sutures are not easily visible except with the aid of a microscope. After the sutures are removed the eye looks entirely normal.

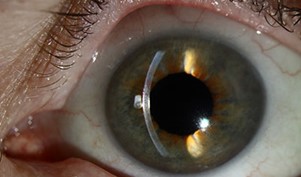
The appearance of the eye three days and one month after DMEK surgery. The cornea is perfectly clear following successful DMEK surgery and the sight is restored to normal
Post-operative care
After the operation, the operated eye will be covered with an eye pad and protective plastic eye shield. As the anaesthetic wears off, some mild discomfort may be felt in and around the operated eye.
Patients undergoing a full thickness corneal transplant or DALK may resume normal activities after about 2 weeks.
Patients having a DMEK or DSEK operation will need to lie flat on their back for 3 hours immediately after the operation. For DMEK patients, some posturing is usually required for the first 2 days post operatively. Normal activities can be resumed after about 2 weeks.
Stiches for full thickness graft and DALK
The very tiny stitches that are put into the cornea hold the transplant in place but also affect its shape and therefore the way the eye focuses. They are not dissolving stiches and will eventually need to be removed.
The exact timing of suture removal varies between individual patients and is decided on an individual basis. We usually remove all sutures within about 18 months of the surgery.
Treatment and Follow-up
Occasional eye drops are usually required for up to 3 years after the operation. It is essential that the eye drop treatment is continued exactly as instructed. These are necessary to ensure that the eye doesn’t get too inflamed, which would cause pain and might damage the transplant. They are also the most important protection against rejection
Steroid drops can have side effects, which must be watched for. They can cause the pressure to rise in the eye, can reduce resistance to infection and with prolonged use can cause cataracts. Therefore, it is very important that patients are examined regularly after corneal transplantation to monitor the treatment.
For the first year following corneal transplantation, it is necessary to attend the clinic approximately every two months. From one year post operatively, the clinic appointments become much less frequent.
Will I see clearly after the operation?
For the first few months after the operation, your vision will fluctuate. This is part of the healing process and you should not expect to have immediate, clear, useful sight. The visual recovery from DMEK tends to occur within 3-6 weeks, unlike following DALK and PK which can take many months. The final visual outcome of PK and DALK is not achieved until all the sutures are removed, which can be up to 18 months postoperatively. At this stage, you might be either glasses or contact lenses to correct the vision.
What is Keratoconus?
Keratoconus is a degenerative disorder of the cornea. The structural stiffness of the cornea is maintained by protein bonds. However, in keratoconus the number of protein bonds is reduced resulting increased elasticity of the cornea and a slowly progressive change in its shape. The shape becomes more conical and the cornea becomes progressively thinner. This leads to gradual blurring of the vision. Keratoconus usually affects both eyes but one eye may be worse than the other. It typically manifests in adolescence and young adults and affects approximately 1 in 2,000 people.
How is Keratoconus treated?
There are a few different treatments for Keratoconus which include:
- Corneal crosslinking (CXL)
- Wearing specially created contact lenses
- Corneal Transplantation
What happens if it is not treated?
If left untreated, scarring may occur and cause loss of transparency of the cornea, resulting in poor vision. Even without scarring, progressive irregularity of the cornea can profoundly blur the sight. For this reason, it is important to perform corneal crosslinking as early as possibly when progression is identified as this nearly always stops further vision loss.
What is corneal crosslinking (CXL)?
Corneal crosslinking is a treatment that can stop keratoconus getting worse. The procedure involves the application of a photosensitive solution (a solution that responds to ultraviolet light) consisting of riboflavin to the cornea which is activated by illumination with ultraviolet light. The riboflavin reacts with the ultraviolet light to create new protein bonds (crosslinks) throughout the cornea, which recovers and preserves some of the cornea’s mechanical strength. If the procedure is performed early enough it can eliminate the need for corneal transplantation and prevent vision from getting worse
How is corneal collagen crosslinking carried out?
Corneal crosslinking is carried out as a day case procedure under local anaesthetic. During the procedure the skin that covers the cornea is removed to allow absorption of the riboflavin solution that is applied to the cornea in drop form for 10 minutes. Next, the cornea is exposed to ultraviolet light for a further 4 minutes. When the cross-linking treatment is finished a pad is put on the eye and kept on for the first night. The procedure is painless and very straightforward. However, for the first 2 days postoperatively the treated eye can be very sore. We recommend that pain killers are taken during this time.
Following corneal crosslinking, patients are monitored annually in the clinic. Other options like specialist contact lenses may be recommended.